Images
Roger Gomis’ team, in collaboration with another two groups in IRB Barcelona’s Oncology Programme, reveal in Nature Cell Biology the genes and mechanisms that allow liver metastasis to colonize the lung.
The breakthrough introduces a new concept of metastasis from metastasis, which may require a distinct clinical treatment to metastases generated from the primary tumour.
The study has been partially supported by the BBVA Foundation, which provides two IRB groups signing this article with structural funds.
A team of scientists led by Roger Gomis, ICREA researcher and head of the Growth Control and Cancer Metastasis Group at the Institute for Research in Biomedicine (IRB Barcelona), has identified the genes that favour staggered colon cancer metastasis. Published on Sunday in the journal Nature Cell Biology, in addition to Gomis, the authors include Angel R. Nebreda, ICREA and BBVA Cancer Research Professor, and Eduard Batlle, ICREA Professor and head of the Colorectal Cancer Lab, both at IRB Barcelona.
Without a previous lesion in the liver there is no lesion in the lung
Of the colon cancer patients that develop metastases, 40% present metastasis first to the liver and later to the lung, always in this clinical order of appearance. Although this staggered behavioural pattern was known, it was not understood at the molecular level.
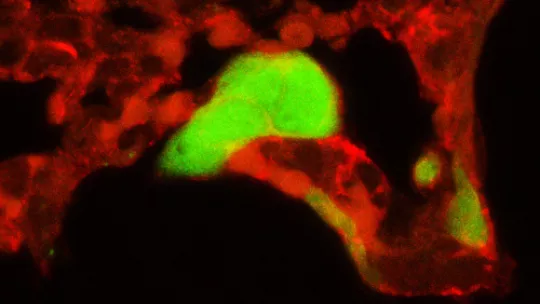
The study reveals that the metastatic lesion in the liver is necessary for later metastasis to lung to occur, the former thus becoming a platform from which the cells prepare the subsequent lung metastatic niche to be colonized. The first authors of the study Jelena Urosevic and Xabier Garcia-Albéniz are postdoctoral researchers with Gomis’ group and the latter is also affiliated to the Hospital Clínic de Barcelona-IDIBAPS.
The key: permeabilize the blood vessels through PTHLH facilitating colonization of the lungs
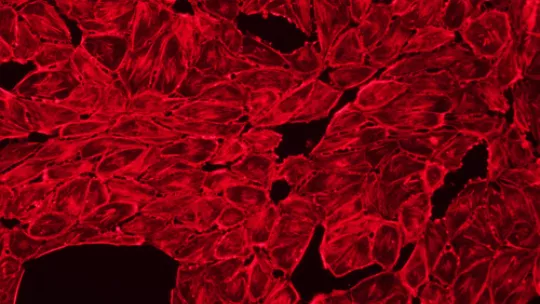
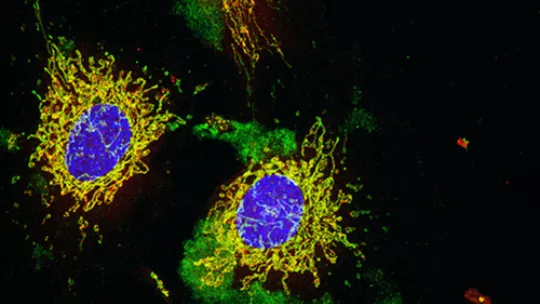
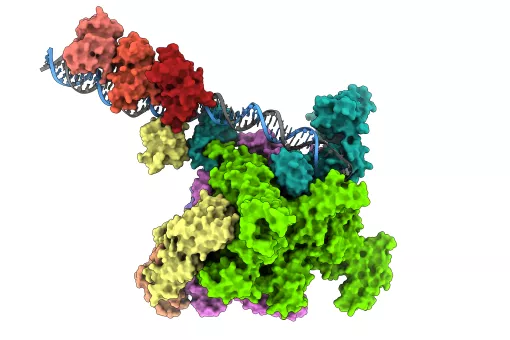
The researchers observed that established metastatic cells in the liver release a molecule called PTHLH. This molecule affects the cells of pulmonary blood vessels, which respond to PTHLH by triggering remodelling processes. When a tumour cells escapes from the liver to travel towards the lung, it releases more PTHLH, thus further stimulating the process. This causes the previously impermeable blood vessel walls to form gaps, which the metastatic cell exploits to cross into and colonize the lung.
“Without the signal from the liver, the tumour cells could hardly enter the lung. With PTHLH, the cells that have colonized the liver are armed with a system that facilitate their activity at a distant site and they are able to prepare a niche in which to generate a new lung lesion. The tumour cells gain capacity to form PTHLH when the levels of p38 MAPKinase are decrease,” explains Roger Gomis.
P38 inhibitors are currently being developed for the treatment of several cancers. “Our results suggest that administering p38 inhibitors to certain patients with advanced stages of colon cancer or with established metastases could be counterproductive and may enhance cell acquisition of lung colonization potential,” says Gomis.
Of note, most patients that develop metastasis to the liver do not do so to the lung, thanks to maintenance—among other factors— of appropriate p38 MAPKinase levels.
The experiments have been validated in 284 clinical samples from patients with stage II and III colon tumours. These are the most relevant cases clinically because they are patients that have not developed metastases but could have acquired this capacity. The results have also been confirmed in cell lines and mouse models.
The groups headed by Gomis and Nebreda receive funding from the BBVA Foundation to conduct studies on cancer and metastasis at IRB Barcelona.
This study has also been made possible thanks to funding from the European Research Council, the Generalitat de Catalunya, and the Spanish Ministerio de Economía y Competitividad. The research has also involved scientists from the Hospital Clínico de Barcelona and the Memorial Sloan Kettering Cancer Center.
Reference article:
Colon cancer cells colonize the lung from established liver metastases through p38 MAPK signalling and PTHLH
Jelena Urosevic, Xabier Garcia-Albéniz, Evarist Planet, Sebastián Real,María Virtudes Céspedes, Marc Guiu, Esther Fernandez, Anna Bellmunt, Sylwia Gawrzak,Milica Pavlovic, RamonMangues, Ignacio Dolado, Francisco M. Barriga, Cristina Nadal, Nancy Kemeny, Eduard Batlle, Angel R. Nebreda and Roger R. Gomis
Nature Cell Biology (2014) DOI: http://dx.doi.org/10.1038/ncb2977
About IRB Barcelona
The Institute for Research in Biomedicine (IRB Barcelona) pursues a society free of disease. To this end, it conducts multidisciplinary research of excellence to cure cancer and other diseases linked to ageing. It establishes technology transfer agreements with the pharmaceutical industry and major hospitals to bring research results closer to society, and organises a range of science outreach activities to engage the public in an open dialogue. IRB Barcelona is an international centre that hosts 400 researchers and more than 30 nationalities. Recognised as a Severo Ochoa Centre of Excellence since 2011, IRB Barcelona is a CERCA centre and member of the Barcelona Institute of Science and Technology (BIST).